Mobile Health Apps: Ensuring Flawless Functionality and Usability for Clinicians and Patients
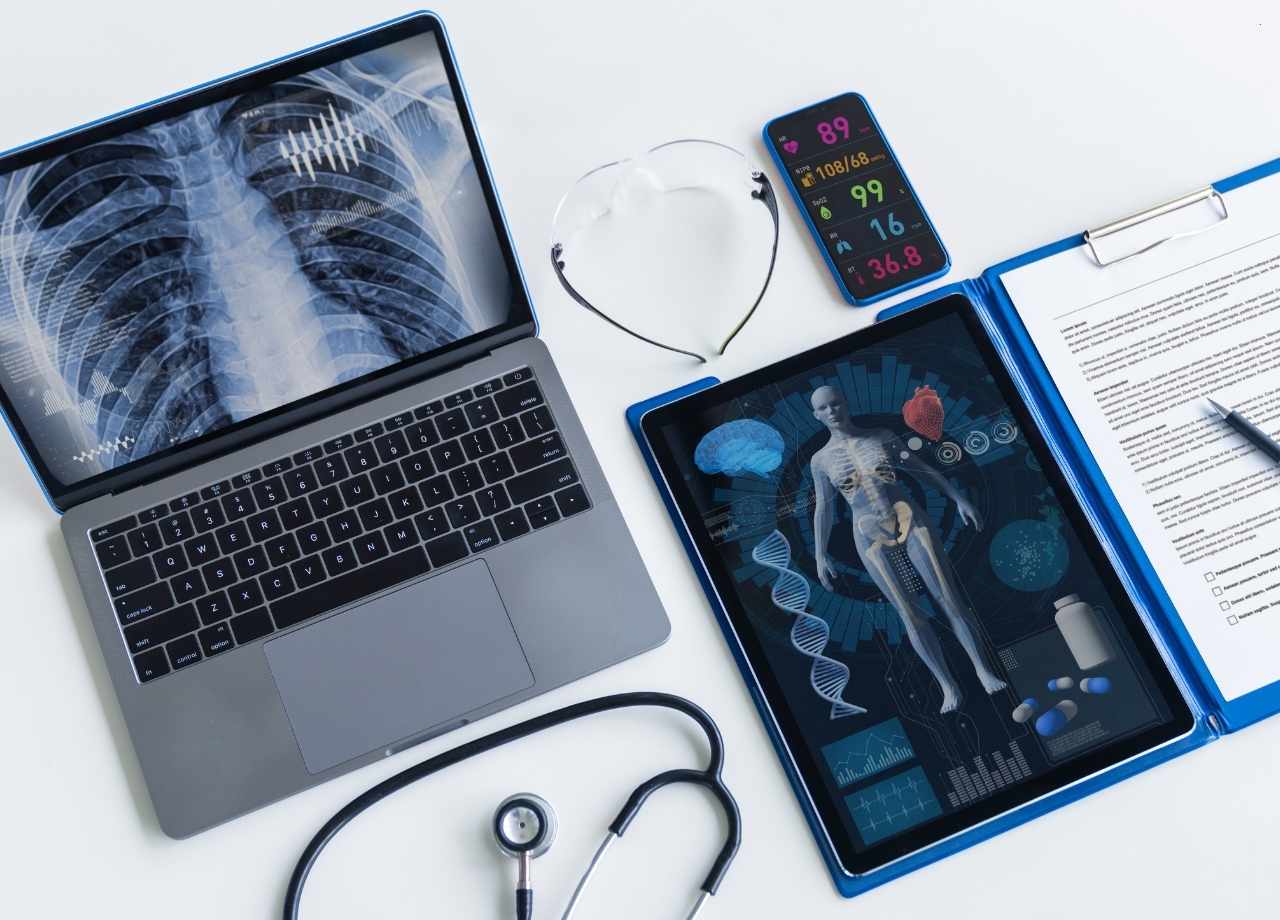
Latest Insights Mobile Health Apps: Ensuring Flawless Functionality and Usability for Clinicians and Patients June 26, 2025 Sajid M. Healthcare Testing In an era where digital transformation is rapidly redefining healthcare, mobile health apps (mHealth) are at the forefront of innovation. From chronic disease management and medication tracking to teleconsultations and diagnostic support, these apps are revolutionizing how patients and clinicians interact. But for all the promise mHealth holds, the execution often falters—not because of poor ideas, but because of inadequate attention to functionality, usability, and quality assurance. At Testiva, we’ve seen firsthand how the smallest bug or usability flaw can cascade into a critical failure—especially in a domain as sensitive and high-stakes as healthcare. That’s why QA testing for mHealth applications isn’t just important; it’s indispensable. Our Functional Testing service has become a key ally to digital health startups and medical software companies looking to launch apps that patients and clinicians can truly rely on. The Critical Intersection of Health and Technology Unlike e-commerce or social media platforms, mHealth apps operate in a domain where data accuracy and interface reliability can have life-altering consequences. A miscalculated dosage, a dropped video consultation, or even a confusing UI can impact patient outcomes and trust. For clinicians, who are often juggling multiple systems while under time pressure, any friction in the app experience can translate into real-world risks. That’s why these applications demand a level of functional and usability integrity that goes far beyond traditional mobile apps. Performance bottlenecks or UI inconsistencies that might be considered minor elsewhere become unacceptable in the context of healthcare. And with regulators tightening their grip on digital health solutions, ensuring compliance through robust QA is not just smart—it’s mandatory. The Double-Edged Sword of Innovation The push for real-time health data, AI-powered diagnostics, and telehealth capabilities is creating more complex mHealth apps than ever before. And while innovation is exciting, complexity introduces greater potential for bugs, performance degradation, and unintended behavior across devices and operating systems. Think about a mobile diabetes management app that connects to a Bluetooth-enabled glucose monitor. If the syncing feature intermittently fails or provides delayed data, users could unknowingly make harmful decisions. Similarly, if a UI doesn’t clearly distinguish between two medications, the user could take the wrong one at the wrong time. To mitigate such risks, comprehensive end-to-end testing across functional scenarios, device ecosystems, and user personas is vital. It’s not just about ensuring the app works—it’s about ensuring it works as expected, under real-world conditions, every single time. Functionality First: The Foundation of Trust Functionality is the bedrock of any mHealth application. But unlike other mobile platforms where a crash might simply be an inconvenience, a functional error in a health app can have legal, ethical, and medical consequences. This is where precision-focused QA plays a pivotal role. QA teams must simulate real-use conditions: unstable internet connections, older device models, background apps running concurrently, and various accessibility settings. Test cases must reflect how clinicians and patients actually behave, not just how developers imagine they will. Additionally, API integrations—whether with EMRs, wearable devices, or third-party pharmacies—must be tested extensively. These integrations are often where silent failures occur, especially under load or when external services change their responses or performance. QA testers need to validate every handshake, data transfer, and failover scenario to prevent functional degradation or data loss. Usability as a Clinical Imperative Usability is not a luxury in mHealth—it’s a clinical imperative. A user-friendly app can improve treatment adherence, reduce user error, and enhance engagement. Conversely, poor usability can lead to incorrect data entry, patient frustration, and even app abandonment. Healthcare providers, in particular, are notoriously time-constrained. If an app requires more than a few taps to accomplish a basic task, it’s already lost ground. A well-designed UI needs to follow the logic of the medical professional or the patient, not the engineer. That means intuitive navigation, consistent design language, and accessibility features that account for vision, dexterity, and cognitive challenges. Conducting usability testing with actual clinicians and patients can uncover critical friction points early. Observational studies, heatmaps, and session recordings help testers understand not just whether a feature works, but whether it makes sense. QA isn’t just about finding bugs—it’s about shaping experience. Data Security and Compliance: Not Optional Data privacy is paramount in healthcare. mHealth apps deal with sensitive personal health information (PHI), making them prime targets for cyber threats and subject to strict regulations like HIPAA in the U.S. and GDPR in Europe. From a QA perspective, this means validating that encryption protocols are functioning correctly, ensuring data is anonymized or masked in transit, and verifying user authentication flows across all platforms. Security testing must be embedded into the QA pipeline, not treated as an afterthought. It’s not just about passing audits—it’s about protecting real people. Additionally, compliance checks need to go hand-in-hand with functionality. For example, if a user requests data deletion per GDPR, does the app really scrub every data point from every backend system? Functional QA must verify these legally required features with the same rigor as any core clinical feature. Continuous Testing in a Continuous World Healthcare doesn’t pause, and neither should your QA processes. mHealth applications are increasingly built using agile and DevOps methodologies, with frequent updates and new feature rollouts. Without continuous testing, teams risk deploying regressions that compromise both user trust and clinical safety. Automated testing can play a critical role here, particularly for regression testing across common workflows. But automation must be paired with exploratory manual testing, especially for new features or complex user flows. QA teams should be embedded early in the development cycle, providing feedback from design to deployment. Testiva’s approach to continuous QA allows teams to release confidently, knowing that core workflows—like prescription refills, appointment bookings, or vital tracking—are validated across devices, OS versions, and user profiles before each launch. Real-World Impact: QA as a Driver of Outcomes The most compelling reason to invest in robust QA for mHealth apps isn’t just technical—it’s human. When apps…